Abstract
Purpose: To evaluate whether modifiable cardiovascular risk conditions and lifestyle factors are associated with increased risk for subsequent ischemic heart disease (IHD) and overall mortality among hematopoietic cell transplant (HCT) survivors.
Methods: Greater than one-year HCT survivors aged ≥20 years, treated from 1970-2010 (n=3,833) were surveyed in 2010-2011 about cardiovascular health and lifestyle factors. Respondents (n=2,360, 61.6%) were then followed longitudinally with annual surveys from 2011-2016 for development of IHD. A series of adjusted models evaluated the relationship (hazard ratio, HR) between conventional cardiovascular risk conditions (obesity, hypertension, dyslipidemia, and diabetes) and lifestyle factors (smoking, fruit/vegetable intake, and physical activity) present at the baseline survey with subsequent IHD and overall mortality.
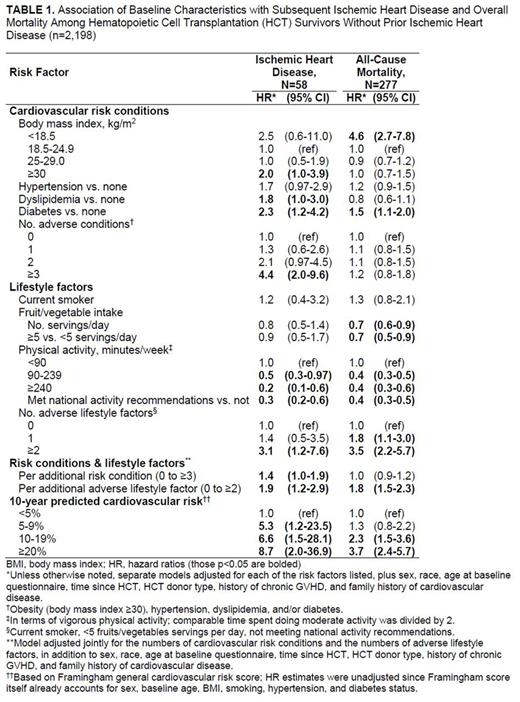
Results: Of the 2,360 HCT survivors (median age at baseline survey, 55.9 years; median time since transplant, 10.8 years), 162 (6.9%) had IHD at time of the baseline survey. Compared with HCT survivors without IHD at the baseline survey, those with IHD had higher rates of hypertension (55.6% vs. 25.8%), dyslipidemia (77.8% vs. 30.6%) and diabetes (34.0% vs. 12.8%), and were less physically active at baseline (54.0% vs. 66.4% met national activity recommendations); p<0.001 for all comparisons. The 5-year overall mortality was markedly higher in HCT survivors with existing IHD compared with those without (28.2% vs. 15.2%, p<0.001). Among those without IHD at time of the baseline survey (n=2,198), the 5-year cumulative incidence of subsequent IHD was 4.3%. Obesity, dyslipidemia, diabetes, and physical inactivity at baseline were all associated with an increased risk for subsequent IHD (Table 1). In contrast, greater physical activity and greater fruit/vegetable intake at baseline were both associated with subsequent reduced overall mortality. When jointly considered, each additional cardiovascular risk condition and each adverse lifestyle factor were independently associated with subsequent IHD (HRs 1.4 [95% CI 1.0-1.9] and 1.9 [95% CI 1.2-2.9], respectively), and adverse lifestyle factors remained associated with overall mortality (HR 1.8 [95% CI 1.5-2.3]). Among those free of IHD at the baseline survey, 492 (23.7%) had Framingham risk scores predicting ≥20% 10-year risk for a serious cardiovascular event, and as expected, those with higher risk scores were more likely to experience subsequent IHD and mortality (Table 1). Overall results remained similar even if HCT survivors who experienced post-HCT relapse were excluded (n=255).
Conclusions: In HCT survivors, cardiovascular risk conditions and adverse lifestyle factors influence the subsequent risk of ischemic heart disease and overall mortality. These results support strong efforts to promote healthy lifestyle behaviors and to treat cardiovascular risk factors more aggressively in HCT survivors. Such efforts may reduce future IHD and overall mortality in this high-risk population.
Flowers: Pharmacyclics: Consultancy. Martin: Fresenius, Neovii: Research Funding; Pfizer: Consultancy; Procter and Gamble: Equity Ownership; Incyte: Consultancy. Lee: Kadmon: Other: One-time advisory board member; Mallinckrodt: Honoraria; Amgen: Other: One-time advisory board member; Bristol-Myers-Squibb: Other: One-time advisory board member.
Author notes
Asterisk with author names denotes non-ASH members.